Key Takeaways:
- ✓Prior authorization is an essential process, but its inefficiencies can disrupt patient care and impact pharmacy revenue.
- ✓Centralizing workflows, improving provider communication, and using technology are key to streamlining PA.
- ✓DocStation provides a range of tools that enhance documentation, compliance, and reporting while simplifying PA management.
- ✓The future of PA lies in interoperability, AI, and the continued shift to value-based care.
- ✓Pharmacies must stay informed of payer-specific requirements and invest in staff training to avoid delays or denials.
Prior authorization (PA) is a gatekeeping process used by payers to ensure the appropriateness of prescribed treatments or medications. Although essential, it creates administrative hurdles that often delay care and increase the workload for pharmacies. Pharmacies need solutions that streamline the PA process while ensuring compliance, efficiency, and timely patient care.
Prior Authorization in Pharmacy Operations
Prior authorization serves as a mechanism for ensuring cost-effective and medically necessary care, but navigating its nuances can be tedious. Here’s how PA works in a pharmacy setting:
- Payer Requirements – Before certain prescriptions are approved, pharmacies must submit documentation proving medical necessity.
- Provider Involvement – Providers are often required to supply supporting information, such as diagnostic codes, therapy history, or lab results.
- Payer Approval – Once submitted, the payer reviews the request, and either approves, denies, or requests additional information.
This process ensures compliance with insurance policies but often delays access to medications, particularly for specialty drugs.
Why It Matters:
- Patients may face interruptions in therapy if PA is not completed promptly.
- Pharmacies risk revenue loss from denied claims or incorrect submissions.
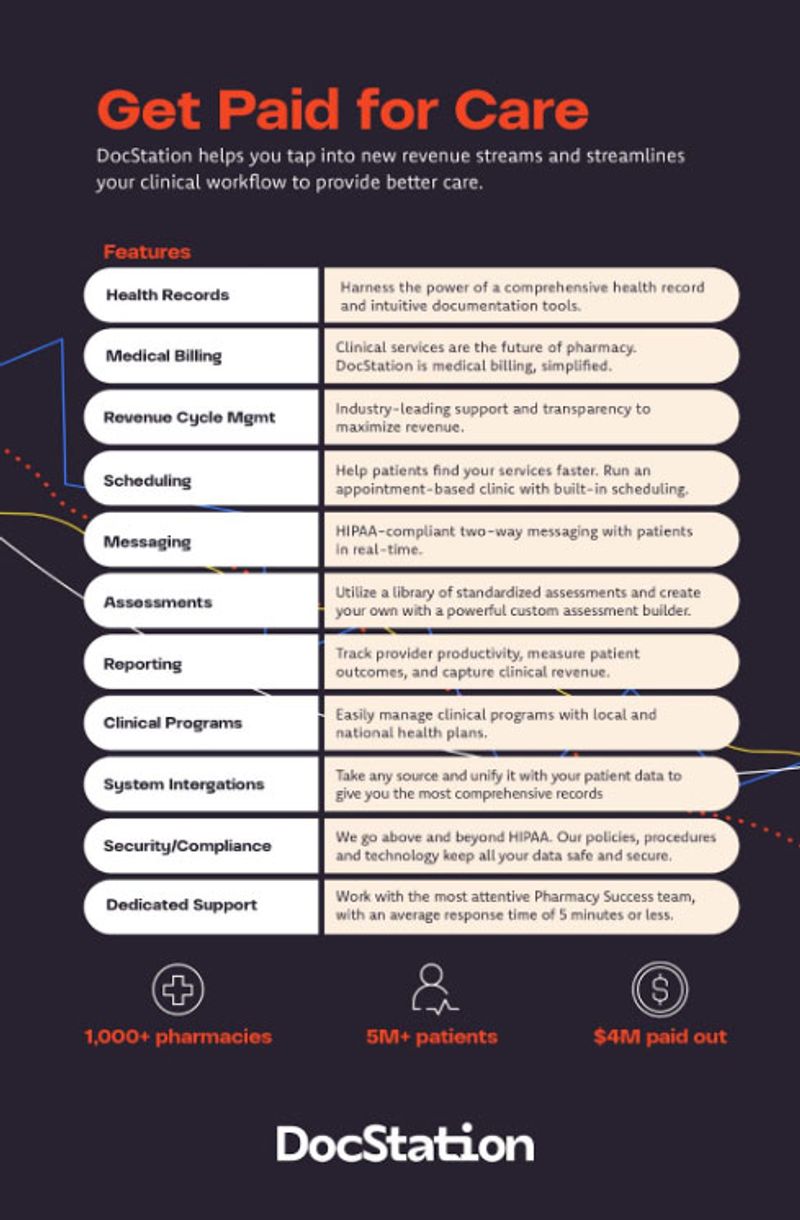
Collaborate, Innovate, Succeed with DocStation
Experience seamless collaboration between providers and payers with our single solution, ensuring pharmacists are fairly compensated for their essential services.
Challenges in the Prior Authorization Process
Prior authorization presents several challenges for pharmacies:
- Time-Consuming Submissions: Completing and submitting forms for each payer is labor-intensive and prone to errors.
- Inconsistent Processes: Each payer has unique requirements, making it difficult to standardize workflows.
- Delays in Communication: Misaligned communication between pharmacies, providers, and payers can result in unnecessary back-and-forths.
- Impact on Patient Experience: Patients waiting for medication approval may experience frustration and interruptions in their treatment plans.
Best Practices for Streamlining Prior Authorization
Centralized Workflow Management
Consolidating all prior authorization requests into one system ensures visibility, reduces errors, and prevents delays in therapy. A centralized system can also incorporate payer-specific requirements, streamlining documentation.

Seamless Coordination with Providers
Efficient PA processes require strong communication between the pharmacy and prescribing providers. To improve coordination:
- Use standardized request forms tailored to payer-specific requirements.
- Proactively notify providers when additional information is needed.
Leveraging Technology for Efficiency
Technology can significantly reduce the administrative burden of PA. Consider using:
- Data Integration Platforms: To consolidate patient and prescription data in one place.
- Automated Documentation Tools: Functionality enabling form completion leveraging available data.
- Submission Tracking Systems: To monitor the progress of PA requests and follow up promptly on denials.
Training and Knowledge Sharing
Train pharmacy staff on payer policies, PA requirements, and technology platforms to ensure compliance and reduce delays. Regular updates on policy changes can also help staff stay ahead of new payer requirements.
“Streamlining prior authorization starts with simplifying workflows, investing in technology, and prioritizing patient care at every step.”
How DocStation Supports Prior Authorization Management
DocStation offers a range of tools to assist pharmacies in managing the prior authorization process more effectively.
Integrated Health Records for Precision
DocStation consolidates patient records from various sources into one centralized health record, ensuring accuracy in documentation and minimizing submission errors. The platform’s focus on centralized data ensures compliance and efficiency.
Scheduling Optimization
DocStation’s open scheduling feature facilitates follow-up reminders, reducing wait times for therapy adjustments or provider communication.
Customizable Assessments and Reporting
Pharmacies can use DocStation’s built-in assessments to standardize data collection for prior authorization submissions. Reporting tools are available track outcomes, measure productivity and support claims reconciliation.
Secure and Compliant Communication
DocStation supports HIPAA-compliant messaging for real-time, secure communication between patients and providers. This ensures ongoing privacy and security of sensitive information throughout the PA process.
“With tools like DocStation, pharmacies can tackle the administrative burden of prior authorization while maintaining compliance and improving financial outcomes.”
Service Authorization in Pharmacy Operations
In addition to medication prior authorizations, pharmacies may encounter service authorizations, which applies specifically to pharmacy-provided services and activities as opposed to medications. Service authorization ensures that clinical services such as Medication Therapy Management sessions, immunization services, point-of-care testing, diabetes education programs, and smoking cessation counseling are appropriately covered under a patient’s insurance benefits.
Additionally, service authorization may apply for specialized equipment and supplies, including durable medical equipment (DME), diabetic testing supplies, continuous glucose monitors, specialty medication supplies, and compounding services. Most commonly, service authorizations are leveraged by payers to manage costs effectively while ensuring patients receive necessary and medically appropriate services.
For example, diabetes self-management education may require a service authorization verifying the pharmacist’s certification, documents supporting medical necessity, service limitations (e.g. two encounters annually), and maximum reimbursement rates.
Streamlining the Service Authorization Process
The service authorization process typically involves several critical steps to ensure compliance and efficient service delivery. Pharmacies must first verify that the desired service is covered under the patient’s insurance benefit and confirm medical necessity. This involves documentation of provider credentials and certifications to provide the service.
Once these pre-requisites are satisfied, pharmacies must obtain insurance approval prior to service delivery, ensuring appropriate encounter coding. Efficient management of service authorizations is essential to prevent delays in patient care and mitigate revenue loss from denied claims.
Similar to managing medication prior authorizations, leveraging technology platforms like DocStation can streamline the service authorization process by centralizing documentation, automating verification steps, and facilitating seamless communication with payers. This not only enhances operational efficiency, but also ensures that patients receive timely and high-quality pharmacy services.
Comparing and Contrasting Prior Authorization and Service Authorization
Both Prior Authorization (PA) and Service Authorization (SA) play an important role in a health plans strategy to manage healthcare costs and ensure medically necessary services. Despite their similarities, PAs and SAs require different distinct operational approaches.
Similarities
Objective of Cost Management and Compliance
Both PA and SA are mechanisms employed by payers to control healthcare expenditures and ensure that the prescribed medications or services are medically necessary and appropriate for the patient’s condition.
Insurance Dependency
Each authorization type requires verification and approval from insurance providers before the pharmacy can dispense medications or provide services, ensuring that the patient’s benefits cover the intended treatment or service.
Documentation and Submission Requirements
Both processes necessitate thorough documentation, including patient information, medical necessity, and relevant clinical data. Accurate and complete submissions are critical to avoid delays or denials.
Impact on Workflow and Revenue
Inefficiencies in either PA or SA can lead to increased administrative burdens, delays in patient care, and potential revenue loss for pharmacies due to denied claims or incorrect submissions.
Differences
Scope of Authorization
- Prior Authorization (PA): Primarily focuses on the approval of specific medications, particularly high-cost or specialty drugs. It ensures that the prescribed medication is necessary based on the patient’s medical condition and treatment history.
- Service Authorization (SA): Pertains to pharmacy-provided services and activities beyond medication dispensing. This includes clinical services like Medication Therapy Management (MTM), immunizations, point-of-care testing, diabetes education programs, and the provision of specialized equipment or supplies.
Process Specifics
- PA: Typically requires detailed clinical justification for the medication, including diagnostic codes, therapy history, and lab results. The focus is on the appropriateness of the drug therapy.
- SA: Involves verifying coverage for specific services or equipment, confirming the pharmacy’s credentials and certifications to provide the service, and ensuring billing codes accurately reflect services rendered.
Approval Criteria
- PA: Approval is based on the necessity and appropriateness of the medication for the patient’s condition, often requiring input from prescribing providers.
- SA: Approval focuses on the necessity of the service or equipment, the provider’s qualifications, and adherence to payer-specific requirements for service delivery.
Streamlining Both Authorization Processes
To effectively manage both PA and SA, pharmacies can adopt several best practices.
Centralized Workflow Management
Implementing a unified system to handle both types of authorizations can enhance visibility, reduce errors, and prevent delays in therapy. . A centralized system can also incorporate payer-specific requirements, streamlining documentation.
Enhanced Communication
Maintaining clear and consistent communication channels with both providers and payers is essential for timely approvals and resolving any issues that arise during the authorization process.
Leveraging Technology
Utilizing advanced platforms like DocStation can automate data collection, standardize payer and service-specific requirements, and promote up-to-date tracking of request status. Leveraging these tools fosters expedited approvals while minimizing administrative burden.
Staff Training and Knowledge Sharing
Regularly pharmacy staff training is essential for PA and SA processes. Ideally, pharmacies should incorporate updates to state regulatory and payer-specific requirements, ensuring team members are equipped to coordinate submission and denial management efficiently and accurately.
By understanding the distinct roles and processes of Prior Authorization and Service Authorization, pharmacies can better navigate the complexities of insurance requirements, ultimately enhancing patient care and optimizing operational efficiency.
The Role of Technology and Future Trends in PA
The future of prior authorization is tied to advancements in healthcare technology, including:
Interoperability
Improved data-sharing standards and implementation between payers, providers, and pharmacies will facilitate a greater degree of process automation and efficiency. For instance, ePA (electronic prior authorization) systems are becoming more common, offering real-time submission and approval tracking.
AI and Predictive Analytics
Artificial intelligence can help pharmacies identify common PA roadblocks and proactively address them. Predictive analytics tools could flag prescriptions that may require prior authorization before submission, saving valuable time.
Value-Based Care Models
As healthcare shifts to value-based care, the reliance on PA for cost control may decrease. Pharmacies can focus on improving outcomes rather than navigating administrative hurdles.
Got Questions? We’re Here to Guide You!
Q1: How long does prior authorization take to process?
PA and SA processing times vary depending on the payer and the complexity of the request. On average, approvals can take anywhere from 24 hours to a week or longer. Tools like DocStation can help track submissions and reduce delays.
Q2: What happens if a prior authorization is denied?
If an authorization is denied, pharmacies should review the denial notes and payer policies, gather missing or incomplete information, and submit an appeal promptly. Proper documentation and follow-up are key to reversing denials.
Q3: Does DocStation automate the entire PA process?
No one system fully automates the PA or SA process. While DocStation supports documentation, reporting, and compliance, it does not offer end-to-end PA automation. Like other systems, DocStation requires hands-on pharmacy staff monitoring and management.
Q4: Can patients track their prior authorization status through DocStation?
DocStation prioritizes secure communication and streamlined workflows. While patients don’t have direct access to prior authorization status or health records, pharmacies can leverage DocStation’s HIPAA-compliant messaging to provide timely updates and ensure patients stay informed throughout the process.
Q5: What are the common reasons for PA denials?
Common denial reasons include incomplete documentation, missing clinical justification, or submitting requests to the wrong payer portal. Implementing standard and centralized processes through systems like DocStation can reduce denials.
Q6: Are there tools that provide real-time PA updates?
While DocStation doesn’t offer real-time alerts, many ePA systems integrated with health plan portals can provide instant updates on submission status.
Simplify Pharmacy Operations with DocStation
Improve patient care and efficiency with DocStation’s seamless provider-payer collaboration.
Efficient prior authorization isn’t just about compliance—it’s about ensuring patients receive timely, high-quality care. By adopting best practices and leveraging platforms like DocStation, pharmacies can meet regulatory demands while improving operational efficiency.