Decoding a technology standard to advance practice.
Breakthroughs in modern medicine have paved the way for antiviral drugs that could help prevent HIV; Researchers have identified methods to grow entire body parts from stem cells; Real-time language translation has been achieved by coupling voice recognition technology with artificial intelligence. These great innovations are changing the world as we know it, all while the healthcare technology industry is simply trying to figure out how to take patient information from one system and transfer it to another.
Exchanging patient information between healthcare settings may not seem like a revolutionary concept, but it has in fact been an ongoing effort for decades; Albeit, we must strive for advancement and innovation in this facet of our healthcare system just as we do elsewhere. The Pharmacist eCare Plan aims to break interoperability barriers, improve chronic disease management, and leverage the unique skill set of Pharmacists as members of healthcare teams.
What Pharmacists Need to Know
The Pharmacist eCare Plan is complex and has many facets. Pharmacists should not be expected to comprehend the technical requirements, implementation specifications, or so called “behind the scenes” logistics of the eCare Plan. However, pharmacists should be expected to speak confidently to the practical uses of the eCare Plan and how it can advance pharmacy practice and business opportunities. It is extremely important to talk directly to software vendors about product roadmaps to ensure their goals align with the goals of the pharmacist’s practice.
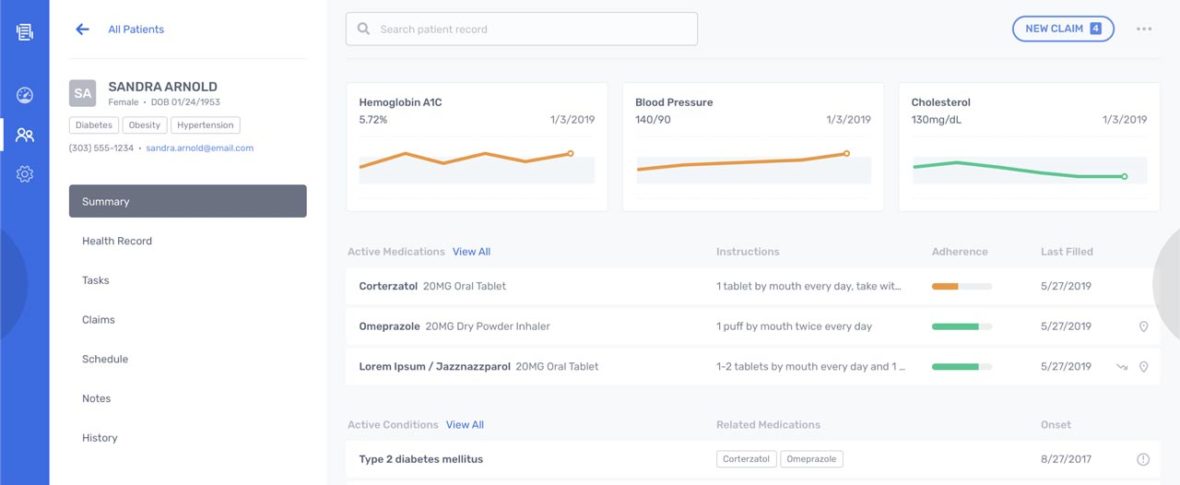
Software companies should design products that maximize pharmacists’ time with patients
Vendors should not only be expected to implement the technical requirements of the eCare Plan, but ensure the products and features are built to support current and future pharmacy workflows. Lack of investment in user experience within EHRs and pharmacy software has contributed to operational inefficiency, patient safety issues, and provider burnout. Software companies should design products that maximize pharmacists’ time with patients and minimize administrative tasks such as documentation and billing. More time with patients.
That that we have that covered, let’s take a closer look.
Healthcare Interoperability
The passing of the HITECH Act in 2009 headed America’s effort to improve communication and ultimately continuity of care across the healthcare industry. This pressured health organizations to work toward the capability of exchanging patient data electronically. Reimbursement from federal programs like Medicare are now partially affected by the capabilities of provider software systems, namely their ability to exchange patient data with other health organizations. This initiative, first coined as Meaningful Use evolved into Promoting Interoperability (PI), applies to all healthcare organizations that provide direct patient care.
These initiatives put most of the pressure on vendors like Epic, Cerner, Meditech, and Allscripts that are contracted by healthcare organizations to provide EHR software. These massive players were never incentivized or required to share data electronically before, so they built their platforms using proprietary data elements, data models, reporting specifications, etc. Needless to say, modifying these already complex platforms with the capability of readily exchanging data with other platforms has proven to be a difficult task.
Interoperability standards have been developed for health organizations and their contracted software vendors to follow in order to ease transitional difficulties. Following these interoperability standards allows health organizations to meet the technological requirements to exchange patient data. Now that the foundational requirements have been established, the focus has shifted from building out data sharing capability to finding the optimal method for conducting data exchange.
Standards for Data Exchange
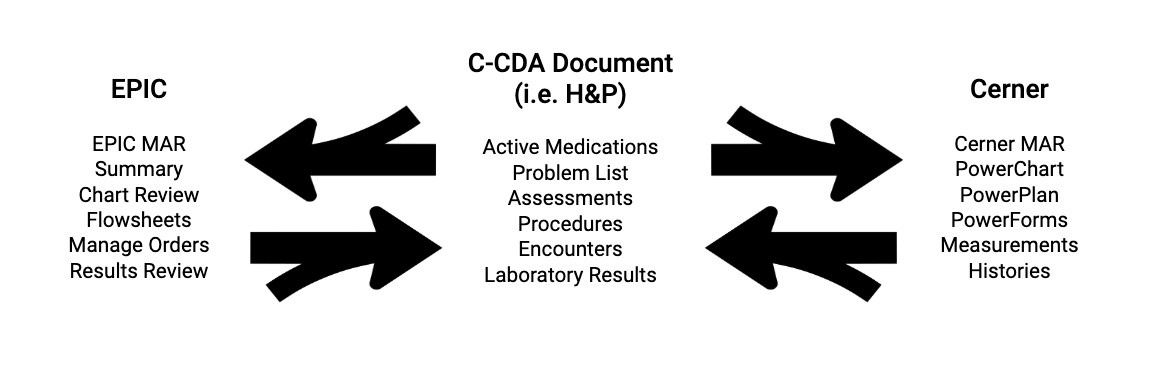
For healthcare data to move from one system to another and remain unchanged, it must be sent in a known, agreed upon format. This standard format, called C-CDA (Consolidated-Clinical Document Architecture) defines how electronic clinical documents should be organized at the data field level so the intended clinical purpose and meaning is preserved during an exchange. Examples of C-CDA documents include the History and Physical (H&P), Continuity of Care Document (CCD), Discharge Summary, and Progress Note. Each C-CDA document contains patient information for a specific use case. For example, the H&P contains background information that is relevant for a routine checkup or hospital admission including the patient’s problem list, allergies, current medications, family history, past procedures, etc.
Think of C-CDA format as a template for each type of clinical document; Understanding this template provides a framework for completely different systems to communicate. Any healthcare organization can exchange data with another if it can pull stored patient data, organize that data into C-CDA documents, and send C-CDA documents. Likewise, organizations must also be able to interpret these documents and store data appropriately within their own EHRs. It matters little where data is stored in any respective system or how it is pulled into documents. What matters is that the system is able to manage data based on the C-CDA framework.
C-CDA and the interoperable formatting standards that came before it opened the door to exchanging health information, but data exchange is still limited to the contents of each C-CDA document. As we transition from C-CDA to the emerging data format standard called FHIR (Fast Healthcare Interoperability Resources), interoperability will improve. FHIR breaks C-CDA format into smaller, more modular packages of data, called resources. FHIR resources are much more robust and incorporate modern standards of the internet. FHIR will open the door to freely exchange not only clinical documents, but all health data.
FHIR will open the door to freely exchange not only clinical documents, but all health data.
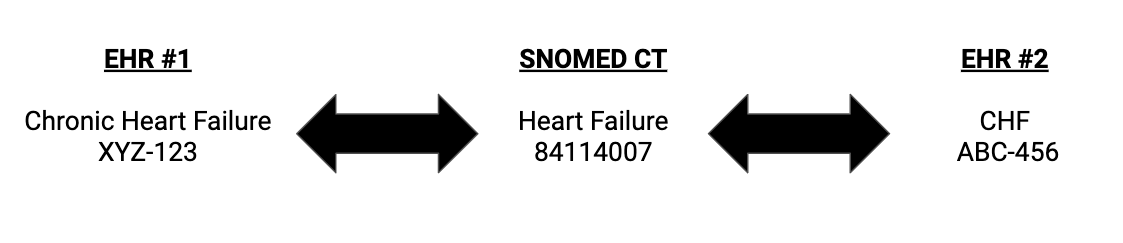
Structuring data in a standard format using C-CDA documents provides a framework for exchange, but systems must also understand the contents of C-CDA documents down to the data element level. For two people to effectively communicate, they must have a common vocabulary; Technology is no different. In health information exchange, this common vocabulary is achieved by establishing massive databases with unique codes assigned to clinical concepts.
SNOMED CT, RxNorm, LOINC, and CVX, are established clinical language standards; all specializing in different types of clinical data, the contents of each vocabulary amounts to millions of codified clinical terms; Systems that assign proprietary, non-standard codes to clinical terms internally can use standard clinical vocabularies as a translator when exchanging data with other systems via C-CDA documents.
Any healthcare organization can interpret and construct C-CDA documents for the purpose of health data exchange as long as their unique internal code system can be mapped to the standard clinical concepts in each C-CDA document, and vice versa. One EHR software is not required to understand the internal code system utilized in another; as long as they both understand standard clinical vocabularies they can exchange data.
The Pharmacist eCare Plan
The Pharmacist eCare Plan is an electronic care plan, but it is much more than that. It contains all the basic information a traditional care plan would related to medication management with additional sections specific to payer information (see below).
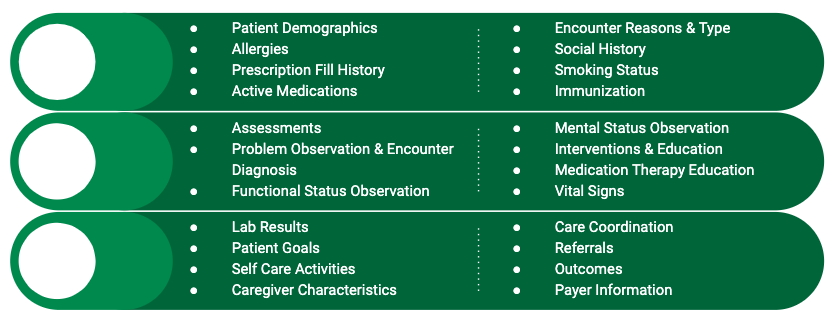
The Pharmacist eCare Plan was built with interoperable data standards to allow for integration with any clinical documentation software used by any health organization. It is structured using the standard format, C-CDA, so it can function just like H&Ps, CCDs, discharge notes, and progress notes. The eCare Plan is even set up and for the future data standard, Fast Healthcare Interoperability Resources (FHIR), when the industry makes the shift.
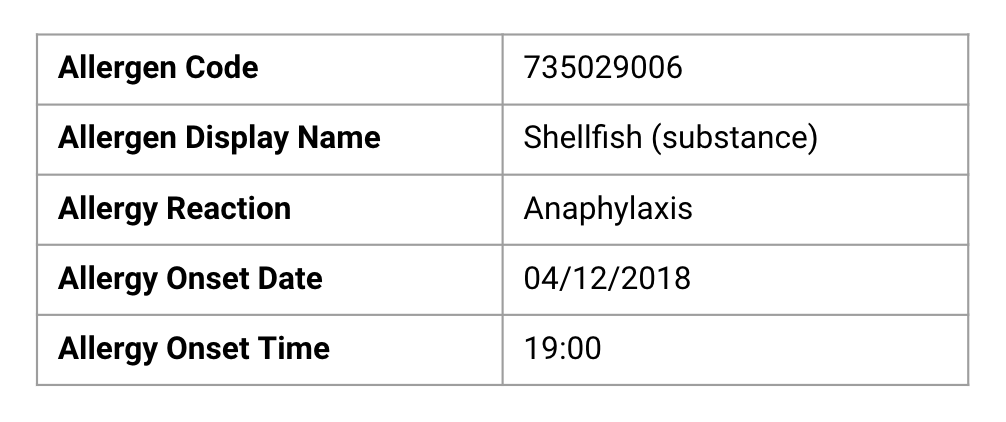
The Pharmacist eCare Plan leverages standardized clinical languages, so any organization anywhere will be able to understand its data contents. Every possible segment of free text and unstructured data in every section of a traditional care plan is replaced with discrete data. Here is the allergies section of the Pharmacist eCare Plan and what it could look like filled out.
The Pharmacist eCare Plan has the potential to capture everything important related to medication management, and because it was built with interoperability data standards, it can go anywhere a patient goes; this makes it an excellent tool for care coordination. This also means that Pharmacists can spend less time re-collecting or re-documenting the same information during every patient encounter and more time can be spent doing what they are great at — caring for patients.
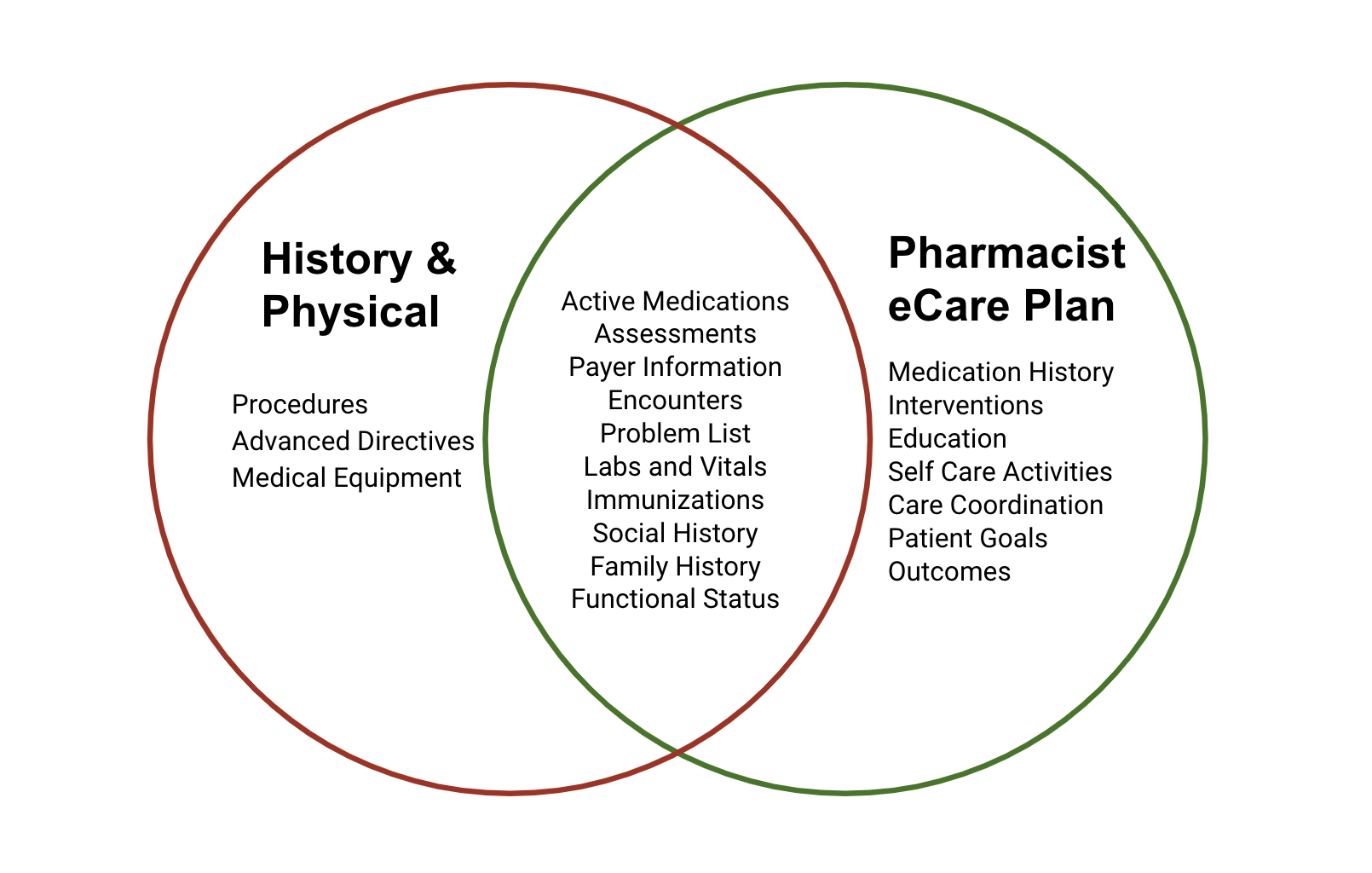
The massive potential for data capture makes the eCare Plan useful for multiple clinical applications and relevant to many providers. Many of the sections that exist in the eCare Plan overlap with sections in other clinical documents. Since C-CDA documents are all built using the same interoperability principles, entire data sections from one document can be pulled into another document that includes the same section. The allergies and medications section of an H&P can be used interchangeably with those sections in the eCare Plan.
It may be called the Pharmacist eCare Plan, but one of the benefits of this electronic document is multi-provider utility. Since Pharmacists are still not recognized under the Social Security Act as providers in most states, their services can not be billed directly to Medicare. Pharmacists play an integral role in health care teams; research has proven that when Pharmacists are involved as members of the health care team, patient outcomes improve, patients report higher rates of satisfaction, and overall health care costs are reduced.
Economic Impact
Americans average less than three ambulatory care visits each year; according to North Carolina Medicaid claims data, a portion of their high risk population visits the pharmacy more than 35 times each year. More direct patient encounters means more opportunities to collect patient information, update active medications, track intervention outcomes, give immunizations, take vitals, obtain lab results, and provide education; all of these interventions are critical in chronic disease management, a facet of our healthcare system that desperately needs attention.
Although the quality of healthcare in America is among the best, we spend more cents on the dollar for health services than almost any other developed country in the world. Americans spend an average $10,000 on healthcare each year while the people living in countries with a comparable health systems spend an average of just over $5,000. There are many factors involved in our overall health expenditure, but one big contributor is chronic disease. Chronic disease accounts for nearly $3 trillion in annual American healthcare spending; It is responsible for around 95% of Medicare spending and 85% of Medicaid spending.
Placing greater focus on the reduction of spending associated with chronic disease could save Americans thousands of dollars each year. The treatment of chronic diseases requires complex medication therapies, and the proper use of medications is essential to preventing disease progression. Pharmacists should be utilized as their comprehensive education and training in medication therapy is unmatched by other healthcare professionals. Their role in care teams managing complex medication therapies is even more important given the impact of inappropriate medication use; 1.5 million preventable medication-related adverse events occur each year in America incurring almost $300 billion dollars in avoidable costs. Medication non-adherence also makes a noticeable dent in our health expenditure, resulting in $100 billion of avoidable costs yearly; Adherence issues contribute to nearly half of the hospitalizations that dialysis patients experience throughout their lives.
Care plans have proven to be imperative for chronic disease management as most chronic disease interventions require ongoing monitoring, periodic assessment, and frequent adjustment. People often suffer from chronic diseases for several decades of their lives, during which unexpected hospitalizations, new healthcare providers, and facility changes are likely to occur; these circumstances require continuity of care. The Pharmacist eCare Plan takes one of the most important tools in chronic disease management and extends its potential to allow for ongoing utilization by multiple providers and health organizations.
The eCare Plan in Practice
There are a few examples of the Pharmacist eCare Plan in use today. The first example is in the Centers for Medicare and Medicaid Innovation Center (CMMI) grant to design, develop, and implement the eCare Plan at Community Care of North Carolina (CCNC). Funded by a CMMI grant, several pharmacy software vendors came together to build and test eCare Plan functionality. CCNC is leveraging the eCare Plan as a billing format. All pharmacies who wish to gain reimbursement for services provided must document and send eCare Plans to CCNC as a record of the encounter. This is a practical example of the eCare Plan used successfully as a business practice.
The Community Pharmacy Enhanced Services Network (CPESN) USA, a joint collaboration between the National Community Pharmacists Association (NCPA) and CCNC, is leveraging the eCare Plan as a reporting standard. CPESN requires all member pharmacies to document in software that supports the eCare Plan and send eCare Plans regularly to CPESN. The goal with this strategy is to compile and aggregate clinical care data from pharmacists providing care across the country and use analytics to support contracting efforts with payers in order to secure payment contracts.
The eCare Plan may also be used to exchange data between providers for care coordination purposes within interdisciplinary teams. The standard allows for this activity to occur, however, it takes both provider organizations to have business incentive to collaborate before a Business Associate Agreement (BAA) is vetted by legal departments and IT resources are appropriated for implementation. To date, there are no documented instances of the eCare Plan used as an interoperability standard to exchange data between pharmacy and EHR systems. Examples should arise in the next few years as pharmacies and health-systems are incentivized to collaborate in value-based care models.
The eCare Plan has vast potential, however, few vendors have the ability to produce an eCare Plan. To further adoption, we must stimulate additional business cases referencing the eCare Plan. For example, the Pharmacy Quality Alliance (PQA) is testing quality metrics that leverage SNOMED CT codes also used in the eCare Plan.
As more organizations adopt standards like SNOMED CT for clinical reporting and the eCare Plan for interoperability, more vendors will be incentivized to offer the eCare Plan as part of their core offering and invest in furthering its capabilities.
Innovations in healthcare data interoperability present an opportunity to improve health outcomes and decrease costs. The Pharmacist eCare Plan targets need in chronic disease management by utilizing a proven tool and expanding its potential use among multiple providers and health organizations. Incorporating the eCare Plan in practice gives pharmacists the opportunity to apply their medication management expertise in chronic disease care teams and assume leading roles in patient care coordination.
**Simon Anderegg, RN, BSN **is a Clinical Systems Analyst at DocStation, a patient care platform for pharmacists.
About DocStation
DocStation gets pharmacies paid for services. Pharmacies use DocStation to provide care, auto-bill medical claims, and participate in value-based programs with innovative health plans.
Get started today and discover how easy it is to get paid for the services you provide every day when you partner with DocStation.