Why DocStation Makes Medicare Part B Billing Effortless (While Other Vendors Leave You Guessing)
Medicare Part B billing for pharmacy services shouldn’t feel like solving a puzzle with missing pieces. Yet for too long, pharmacy providers have struggled with the complexities of determining the right payer, validating coverage, and ensuring claims are submitted correctly the first time.
That changes today.
DocStation has revolutionized Medicare Part B billing with three breakthrough features that eliminate the guesswork and manual work that plague other platforms. Here’s how we’re making Medicare billing not just easier, but actually effortless.
🎯 CMS Payer Predictor: No More Medicare Roulette
Gone are the days of wondering whether your claim should go to the local Medicare carrier or the DME MAC. Our new CMS Payer Predictor with CMS PCN automatically determines the correct Medicare contractor for every claim.
Here’s how it works:
- Simply bill to DocStation’s BIN with the PCN “CMS”
- DocStation automatically maps your NDCs to the appropriate HCPCS codes
- Our AI verifies whether that HCPCS should be submitted to the local Medicare carrier or the DME MAC
- The claim generated in DocStation will automatically be set to bill the exact payer name and PCN you get back in the response, so you’ll know the determination (e.g., “MEDICARE DME MAC JURISDICTION A (2389)”)
The result? Zero guesswork. Zero claim routing errors. Maximum reimbursement efficiency.
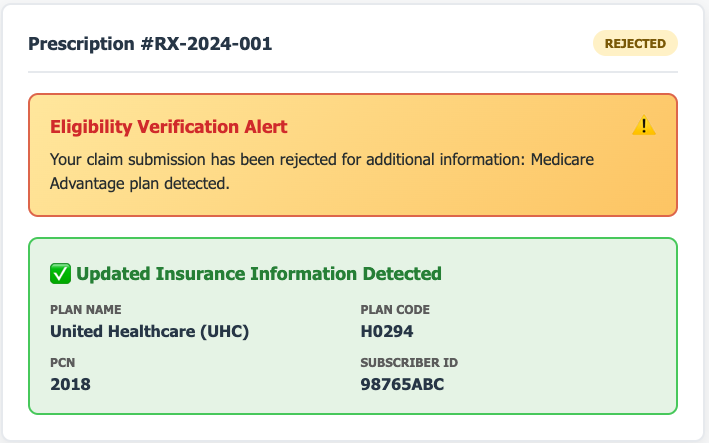
🔍 Enhanced Pass-Back Eligibility: The Medicare Advantage Game-Changer
While other vendors offer basic eligibility checking, DocStation’s enhanced pass-back eligibility feature goes far beyond the competition with Medicare Advantage detection that no other vendor can match.
What makes us different:
- Automatic Medicare Advantage coverage detection with Part B and MA plan verification
- Subscriber ID validation – we show you the relevant subscriber ID information that other platforms can’t access
- Enhanced rejection messages with specific coverage details when needed
- Seamless claim generation – when eligibility is confirmed, BIN billed claims are automatically “paid” and generate medical claims
The competitive advantage: Other vendors leave you in the dark about Medicare Advantage coverage details. DocStation illuminates the entire picture, giving you the information you need to bill correctly every time.
⏰ Smart DME Span Dates: Automation That Actually Works
Manual calculation of service span dates for DME items is not only time-consuming—it’s error-prone. DocStation eliminates this entirely with intelligent automation.
Our system automatically:
- Calculates span dates on applicable DME items
- Uses days supply and quantity dispensed to determine accurate date ranges
- Maps modifiers from pharmacy claims onto medical claims
- Applies predefined rules through our CPT Variants Dataset
The impact: What used to take manual calculation and verification now happens instantly and accurately, reducing claim rejections and accelerating payment.
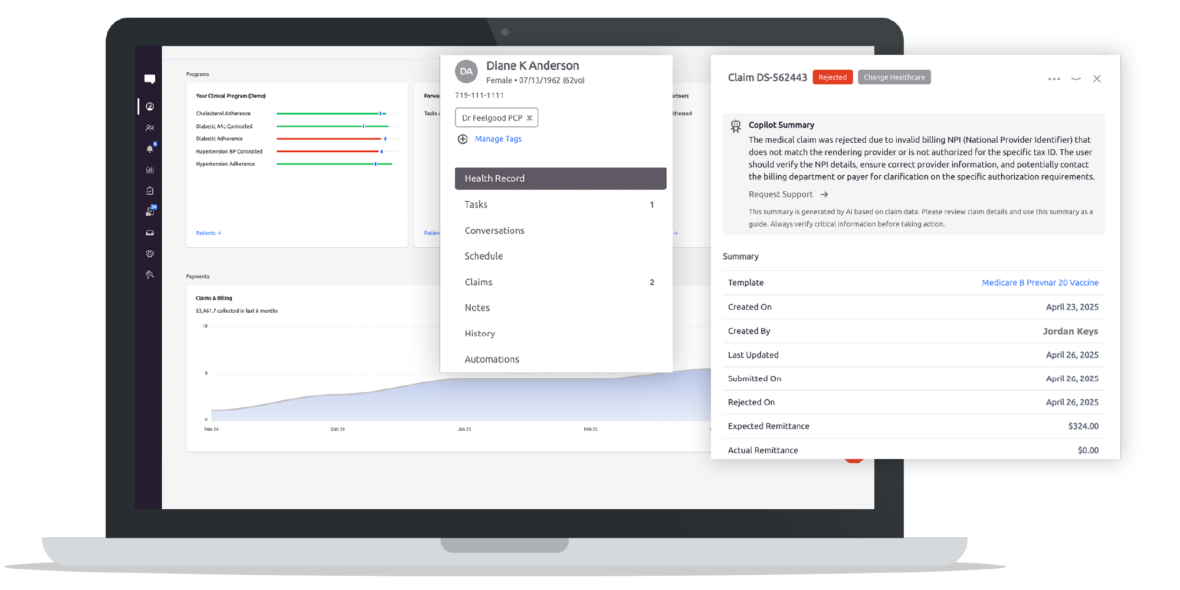
🏥 The DocStation Difference: Built for Modern Pharmacy Practice
These features aren’t just incremental improvements—they represent a fundamental shift in how Medicare Part B billing should work. While other vendors require you to navigate complex workflows and make educated guesses, DocStation provides:
- Intelligent automation that handles the complexity behind the scenes
- Comprehensive coverage detection that reveals what others can’t see
- Accurate claim routing that eliminates the trial-and-error approach
- Seamless integration that works with your existing pharmacy workflows
💡 Real-World Impact: What This Means for Your Pharmacy
For vaccine administration: Our NDC-to-HCPCS mapping ensures seasonal vaccines like influenza, COVID, and RSV are billed with the correct HCPCS codes for each vaccine season, while maintaining up-to-date seasonal formulations—critical for payment within Medicare’s strict seasonal vaccine windows.
For DME services: Automatic span date calculation and Medicare contractor determination mean your DME claims process smoothly without manual intervention.
For Medicare Advantage patients: This is where DocStation’s advantage becomes crucial. With Medicare Advantage enrollment now reaching 54-55% of all Medicare beneficiaries—over 34 million Americans—and continuing to grow every year, the risk of incorrectly billing vaccines to traditional Medicare Part B for Advantage-covered patients has never been higher. Our enhanced eligibility detection provides the coverage insights you need to bill appropriately, whether to traditional Medicare or MA plans, preventing costly claim rejections and ensuring proper reimbursement.
🚀 The Bottom Line
Other vendors treat Medicare Part B billing as a necessary complexity you have to manage. DocStation treats it as a problem we’ve solved for you.
With automatic payer determination, enhanced Medicare Advantage detection with subscriber ID access, and intelligent DME span date calculation, DocStation doesn’t just make Medicare billing easier—we make it effortless.
Ready to experience Medicare Part B billing the way it should be? Contact our team at support@docstation.co to see how DocStation can transform your pharmacy’s billing efficiency and accuracy.