Case Study
Clinical Services
DocStation Clinical Pharmacy Program
Medicare Advantage Health Plan
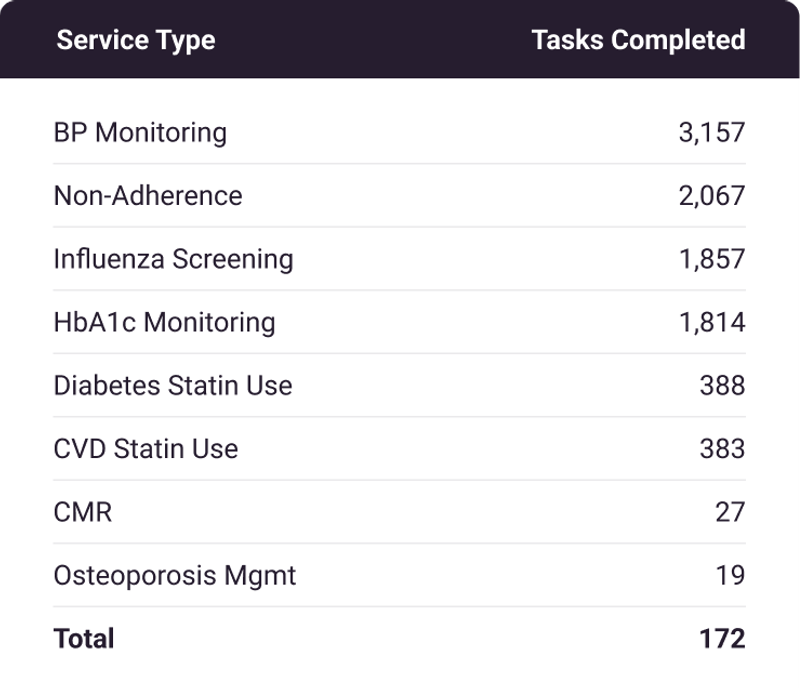
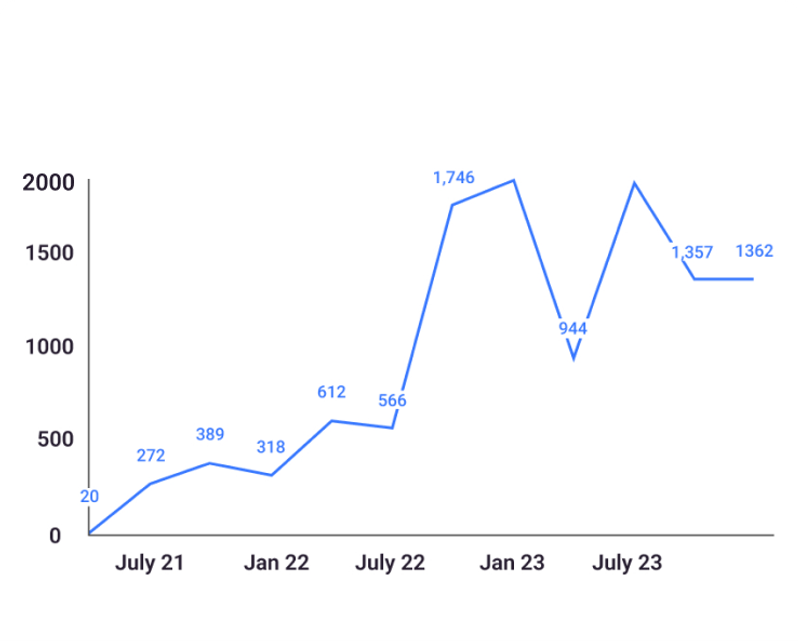
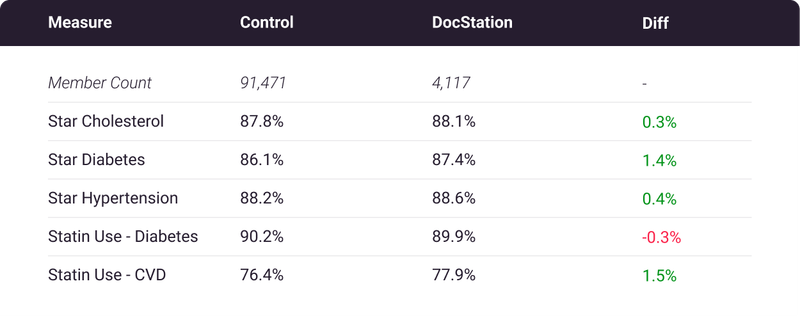
How DocStation's clinical pharmacy program connected 172 pharmacies across 4 states to serve nearly 10,000 Medicare patients with a 72.4% success rate while maintaining 5-star quality ratings.
9,712
Encounters
Total encounters completed since launch
72.4%
Success Rate
Of attempted member engagements
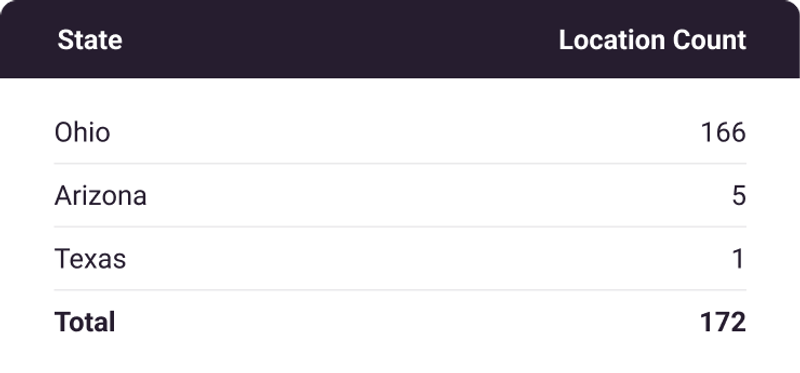
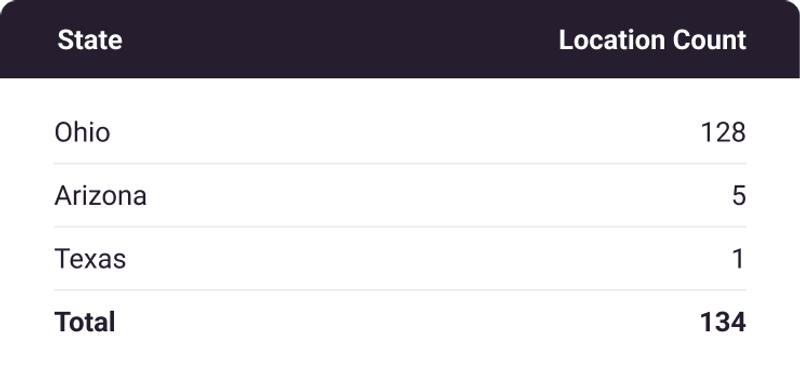
172
Network Size
Pharmacies across 4 states
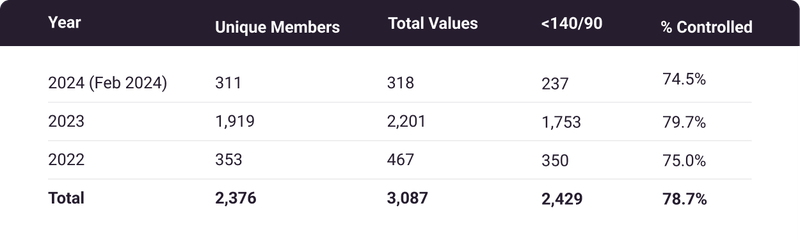
78.7%
BP Control
Blood pressure values within CMS parameters (4-star)
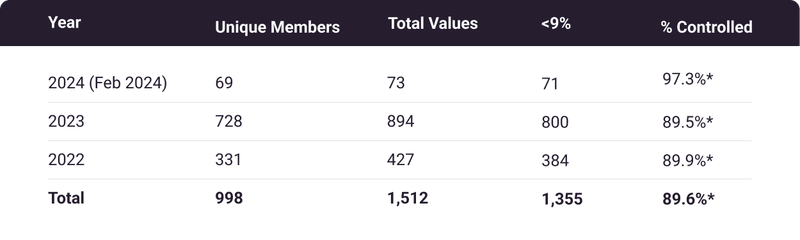
89.6%
HbA1c Control
HbA1c values within CMS parameters (5-star)
$56.62
Cost/Encounter
Program cost efficiency
More Success Stories
Related Case Studies
Clinical Services
A Tech-Enabled Value-Based Program to Reduce Total Cost of Care
Midwest Part D Sponsor
30,000Interventions
Read Case Study
Independent Pharmacy
Pharmacy Earns $70,000 in First Year with DocStation
California Independent Pharmacy
$70K+First Year Revenue
Read Case Study
Independent Pharmacy
Texas Pharmacy Nets $19,000 in First Month using DocStation Billing Automation
Austin, Texas Pharmacy
$19KFirst Month Revenue
Read Case Study